 To have your general questions answered, please email: [email protected]
To have your general questions answered, please email: [email protected]
What is Familial Hypercholesterolaemia (FH)?
Familial hypercholesterolaemia (pronounced hyper-cholesterol-ee-me-ah) usually called FH for short, literally means ‘families with high cholesterol’. FH is an inherited disorder, which means it is passed down from parent to child and often FH (or early heart attacks/death) can be traced over several generations. See Typical family tree.
FH causes very high LDL cholesterol (‘bad’ cholesterol) from birth and will continue throughout life unless diagnosed and treated. This results in an increased risk of cardiovascular disease, specifically coronary artery disease (disease of the arteries of the heart) at an early age.
Early age is defined as men before the age of 55 and women before the age of 60.
People without FH tend to start getting high LDL cholesterol in middle age and take several decades to develop coronary artery disease. If you have FH this process starts at birth and means you can develop coronary artery disease as early as your 20s and 30s. When you have FH, heart attacks at such an early age are not uncommon. Sometimes these heart attacks are fatal.
Early diagnosis and treatment of FH can delay or prevent cardiovascular disease and early death.
How is FH diagnosed?
People with FH:
- have high LDL cholesterol from birth
- have other family member/s with high LDL cholesterol (definitely a parent, 50% siblings and 50% children), see Typical family tree.
- may have cardiovascular disease*¹ at an early age*²
- may have a close family member, who has had cardiovascular disease*¹ at an early age*²
- may have visible cholesterol deposits around the body.
*¹Cardiovascular disease can be: heart attack, stroke, angina, stent, coronary artery bypass graft surgery (CABG) or other circulation problems.
*²Early age is defined as men before the age of 55 and women before the age of 60.
If you think you and your family have FH, you should see your doctor or healthcare provider. A small sample of blood will be taken and the cholesterol levels measured. Your doctor will also do a simple examination and ask for details of your family history (other family members with cardiovascular disease). You may be referred to a specialist lipid clinic, usually in a hospital outpatient department, that deals with cholesterol disorders for further tests, including genetic testing.
How can FH be treated?
FH is treated by lowering LDL cholesterol levels. This can be done by following a healthy lifestyle along with taking medication.
Why is treating high LDL cholesterol so important?
If there is too much LDL cholesterol in the blood, it can deposit in the walls of the arteries giving rise to cardiovascular disease causing heart attacks, stroke and other circulation problems.
Is there a cure for FH?
There is currently no cure for FH, so life-long treatment is required.
How did I get FH?
You inherited one ‘faulty’ LDL receptor gene from one of your parents (the most common form), so 50% of your LDL receptors don’t work; you have heterozygous FH.
Will my children have FH?
The same way you inherited FH so will your child/children.
You have one ‘faulty’ LDL receptor gene (F) and one normal gene (N).
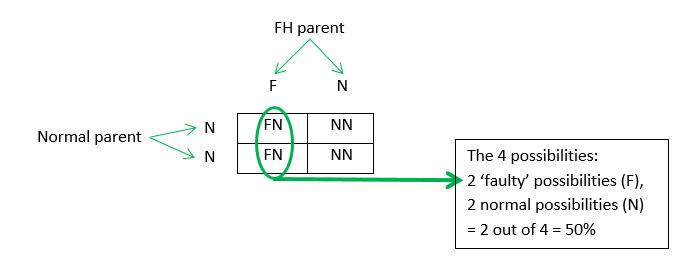
There is a 50% chance that any child will get the ‘faulty’ gene (F) i.e. if you have 4 children, two are likely to have FH.
FH is an autosomal dominant disorder which means if you have the ‘faulty’ gene you have FH.
I have seen a lot of negatives things about statins. Are they necessary, are they safe?
The benefits of statins are greatest in people with heart disease or other risk factors for heart disease, such as FH, diabetes and high blood pressure.
Statins have been shown to be highly cost-effective medication that decrease suffering and disability related to heart disease, as well as saving lives and government expenditure on healthcare. They have a long safety record and are well tolerated. Like every drug, statins do have side-effects, the most frequently reported (5 to 10 % of users) being muscle pain and tiredness. These respond well to lowering the dose of the statin, to switching statins and to supplementing the diet with co-enzyme Q10, fish oils or vitamin D. Most people with this initial side-effect can continue to be treated with a statin with no further symptoms.
There has also been concern about an increase incidence of diabetes, but this is usually seen with higher doses of statins and in people who already have a predisposition to diabetes, such as obesity and slight elevation in blood glucose levels.
The benefits of statins far outweigh the side-effects. People prescribed statins should not stop them without consulting their doctor. Stopping a statin if you are known to have heart disease or have a predisposition to heart disease (FH, diabetes, high blood pressure), may lead to a heart attack.
